Understanding Your TCM Diagnosis:
A friendly guide to what your practitioner writes in your notes—and what it means for you.
What Does “Diagnosis” Mean in TCM
In Traditional Chinese Medicine (TCM), your diagnosis isn’t a disease label like “migraine” or “IBS”. Instead, it’s a pattern—a snapshot of how your body’s systems are functioning right now. Patterns help explain why symptoms appear together (e.g., headaches, premenstrual syndrome, bloating) and point to the most effective treatment strategies.
Think of it like a weather report for your body: is it too hot or too cold? Too dry or too damp? Is there enough energy (Qi) flowing smoothly, or is something obstructing it?
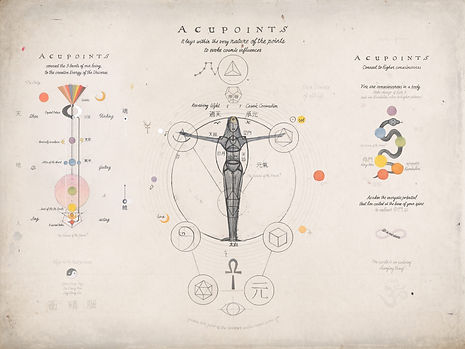
Foundational TCM Concepts Explained
Frequently Seen Patterns in Clinic
These are brief sketches of TCM patterns we commonly see in clinic. They’re not disease labels—they describe the overall “feel” of how your system is working right now. You might recognise yourself in more than one pattern, and that’s normal. Patterns can shift with stress, sleep, your cycle and treatment, so your plan may change as you do.
Liver Qi Stagnation: tight shoulders, sighing, mood swings, PMS, bloating that worsens with stress.
Spleen Qi Deficiency: tired after meals, bloating, loose stools, sugar cravings, “heavy” limbs, brain fog.
Kidney Yang Deficiency: cold hands/feet, low back/knee ache, low morning energy, frequent urination.
Kidney Yin Deficiency: night sweats, dry mouth at night, light sleep, and afternoon fatigue.
Blood Deficiency: light-headedness, dry skin/hair, scanty periods or delayed cycle, trouble focusing.
Damp or Phlegm: persistent congestion, sticky stools, feeling heavy or puffy, “stuck” emotions.
Heat (often from stagnation or deficiency): irritability, red eyes/face, thirst, acne, restless sleep, vivid dreams.
These are patterns, not life sentences. As your body changes, your pattern—and treatment—will change too.
How Your Pattern Guides Care
Your practitioner combines acupuncture, self-care, and lifestyle and dietary advice to tailor a treatment plan that matches your unique pattern.
If you’re stagnant (e.g., Liver Qi Stagnation), we focus on movement—needling that “moves Qi,” breathwork, gentle exercise, and stress-reduction techniques.
If you’re deficient (e.g., Spleen Qi Deficiency): we support and rebuild—steadier meals, warm cooked foods, realistic rest, points that “tonify”.
If there’s heat, we clear and cool—reduce spicy/alcohol/, and sugary foods, improve sleep timing, and use cooling points/herbs where appropriate.
If there’s dampness, we dry and drain—simplify the diet for a while, maintain steady mealtimes, and support gut and lymphatic flow.
Understanding TCM Organ Networks
TCM organ names represent functional networks that encompass emotions, circulation patterns, digestion, and other related aspects. Your TCM diagnosis doesn’t replace medical tests. We always encourage appropriate GP checks and investigations.
How to Use Your Diagnosis Between Sessions
Track 2–4 anchor symptoms (e.g., sleep quality, energy on waking, digestion/bloating, pain score). Note small wins.
Match self-care to your pattern (examples below).
Keep meals regular to support Spleen Qi (your digestive engine).
Move gently, often to prevent stagnation—think walks, stretching, breath-led mobility.
Prioritise sleep—consistent times help both Yin and Qi.
1
Share changes (good or bad) so we can refine your plan.
Your Pattern, Your Plan
Here are practical, bite-sized ideas matched to each TCM pattern. Use them as starting points between sessions—small shifts in meals, sleep, movement and stress usually make the biggest difference. Personalise with your practitioner, especially if you’re pregnant, on medication or managing a medical condition.
Liver Qi Stagnation: daily 10–20 min gentle movement; slower exhale breathing; reduce alcohol; schedule mini “de-stress” breaks.
Spleen Qi Deficiency: warm, cooked foods; protein at each meal; avoid over-snacking; keep feet/abdomen warm.
Kidney Yang Deficiency: morning light exposure; keep lower back warm; steady, warming meals; avoid late nights.
Kidney Yin Deficiency: earlier wind-down, screens off; hydration through the day; cooling, moist foods (pear, cucumber, soups).
Damp/Phlegm: simplify—less ultra-processed/snacking; add gentle sweating through brisk walking; consider short-term dairy/sugar reduction if advised.
Heat patterns: build a calming evening routine; moderate spicy/fried foods; try brief mind-cooling practices (legs-up-the-wall, box breathing).
Always personalise with your practitioner—especially if you’re pregnant, trying to conceive, on medication, or managing a medical condition.
*These self-care ideas are for general information only and are not medical advice. Always personalise with your practitioner—especially if you’re pregnant, trying to conceive, on medication, or managing a medical condition.
FAQs
Can patterns overlap?
Yes. You might see “Liver Qi Stagnation with Spleen Qi Deficiency” or “Kidney Yin & Yang Deficiency”. We treat in layers.
Why did my diagnosis change this week?
Because you changed—stress, sleep, cycle, diet, illness and progress all shift your presentation. Updating the pattern keeps treatment targeted.
Is acupuncture safe?
When delivered by a trained practitioner, serious side-effects are rare. Mild effects (tiny bruises, temporary light-headedness, a short-lived symptom shift) can occur. Tell us if you’re on blood thinners, have a bleeding disorder, or are pregnant.
When should I see my GP urgently?
New chest pain, severe shortness of breath, sudden weakness/numbness, high fever, black/tarry stools, or any symptom that feels alarming or rapidly worsening.
